Dr. John Frattarelli is one of the world’s leading experts on In Vitro Fertilization. Having treated patients for over 20 years, Dr. Frattarelli is the most experienced IVF providers in Hawaii having personally overseen more than 30,000 fertility treatment cycles that have resulted in more than 15,000 babies born.
Dr. Anatte Karmon completed her Reproductive Endocrinology and Infertility Fellowship at Massachusetts General Hospital /Harvard Medical School. Together with Dr. Frattarelli, they offer expert fertility and IVF services to all of Hawaii, the Pacific, and Asia. Drs Frattarelli and Karmon see and treat fertility patients on the island of Oahu (Honolulu and Kailua), Big Island (Hilo and Kona), and Maui (Kahului).
All IVF services in Hawaii are performed in our IVF laboratory in Honolulu at the Fertility Institute of Hawaii. This state-of-the-art Fertility center was founded by Dr. Frattarelli in 2011. The Fertility Institute of Hawaii is able to perform all services related to reproduction. Dr. Frattarelli is one of only a few physicians nationally who also is certified as an HCLD (High Complexity Laboratory Director) for the IVF Laboratory. This allows him to provide singular oversight for all Clinical and Laboratory aspects of the IVF practice. This singular oversight is most likely the reason for the tremendously high pregnancy rates that the fertility practice is able to achieve.

The IVF laboratory of the Fertility Institute of Hawaii has been awarded an accreditation by the Commission on Laboratory Accreditation of the College of American Pathologists, based on the results of an on-site inspection. The accreditation indicates that our laboratory is one of an exclusive group of reproductive laboratories around the country that have met the highest standards of excellence.
CAP is widely considered the leader in quality assurance. The CAP Laboratory Accreditation Program is an internationally recognized program that helps laboratories achieve the highest standards of excellence to positively impact patient care. The goal of the CAP Laboratory Accreditation Program is to improve patient safety by advancing the quality of pathology and laboratory services through education, standard setting, and ensuring laboratories meet or exceed regulatory requirements. CAP inspectors also examine the entire staff’s qualifications, the laboratory’s equipment, facilities, safety program and record, as well as the overall management of the laboratory.
Introduction: In vitro fertilization and embryo transfer (IVF-ET) was first successfully used in humans over 30 years ago; since then, more than one million children have been conceived using this technology. IVF is a procedure designed to enhance the likelihood of conception in couples for whom other fertility therapies have been unsuccessful or are not possible. It is a complex process and involves multiple steps resulting in the insemination and fertilization of oocytes (eggs) in our laboratory. The embryos created in this process are then placed into the uterus for potential implantation. Each stage of the procedure is associated with specific risks, as outlined below.
In Vitro Fertilization is commonly referred to as IVF. IVF is the process of fertilization by manually combining an egg and sperm in a laboratory dish. When the IVF procedure is successful, the process is combined with a procedure known as embryo transfer, which is used to physically place the embryo in the uterus.
There are basically six steps in the IVF and embryo transfer process which include the following:
Step 1: Fertility medications are prescribed to control the timing of the egg ripening and to increase the chance of collecting multiple eggs during one of the woman’s cycles. This is often referred to as ovulation induction. Multiple eggs are desired because some eggs will not develop or fertilize after retrieval. Egg development is monitored using ultrasound to examine the ovaries and blood test samples to check hormone levels.
Step 2: The eggs are retrieved through a minor surgical procedure which uses ultrasound imaging to guide a hollow needle through the pelvic cavity. Sedation and local anesthesia are provided to remove any discomfort that you might experience. The eggs are removed from the ovaries using the hollow needle, which is called follicular aspiration. Some women may experience cramping on the day of retrieval, which usually subsides the following day; however, a feeling of fullness or pressure may last for several weeks following the procedure.
Step 3: Sperm, usually obtained by ejaculation is prepared for combining with the eggs.
Step 4: In a process called insemination, the sperm and eggs are placed in incubators located in the laboratory which enables fertilization to occur. In some cases where fertilization is suspected to be low, intracytoplasmic sperm injection (ICSI) is used. Through this procedure, a single sperm is injected directly into the egg in an attempt to achieve fertilization. The eggs are monitored to confirm that fertilization and cell division are taking place. Once this occurs, the fertilized eggs are considered embryos.
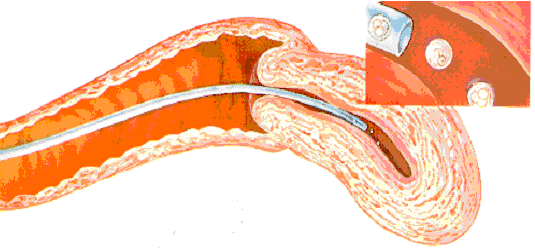
Step 5: The embryos are usually transferred into the woman’s uterus anywhere from two to six days later. At this point, the fertilized egg has divided to become a two-to-four cell embryo. The transfer process involves a speculum which is inserted into the vagina to expose the cervix. A predetermined number of embryos are suspended in fluid and gently placed through a catheter into the womb. This process is often guided by ultrasound.
Step 6: Watching for early pregnancy symptoms. A blood test and potentially an ultrasound will be used to determine if implantation and pregnancy has occurred.
In a normal menstrual cycle, just one egg/oocyte each month develops and matures. The egg matures with a fluid filled structure on the ovary called a “follicle” which can be seen on ultrasound. In an ART cycle, ovulation induction medications (typically daily self-administered injections) are used to stimulate the ovaries so that multiple follicles (eggs) will develop.
Depending on your stimulation protocol, you may begin your first medication in the menstrual cycle preceding the IVF cycle. Then, after your next period, the ovulation induction hormones are begun. Exact instructions regarding their use will be given to you at that time by the staff. These medications will be used for approximately 8 to 12 days, depending upon how your ovaries respond. These medications and their use will be explained in detail before each cycle.
When the majority of follicles have reached a mature size, another medication, human chorionic gonadotropin (hCG), will be given by injection. The hCG must be given at the appropriate time of follicle development to prepare the egg for removal from the body.
Beginning around cycle day 3, we will draw blood samples every 1 to 3 days to monitor the level of estradiol (a form of estrogen) in your blood. These blood tests will be used to determine if estradiol levels are in the range that we would expect prior to ovulation.
Ultrasound monitoring of the ovaries will also be used to follow follicular growth. The ultrasound machine works by sending out sound wave signals which reflect off different structures in the pelvis and give an image of follicles growing on each ovary. When indicated by your hormone levels, ultrasounds will be performed daily as well.
Because ultrasounds are performed using a vaginal probe, you do not have to fill your bladder for this procedure. There have been no harmful effects to developing oocytes or early pregnancy from ultrasound. Monitoring and daily decisions about your care are made by Dr. Frattarelli.
When ultrasound and blood estradiol levels indicate that the follicles are maturing, you will be instructed to give the hCG injection in the evening. You will be told the specific day and time to give your hCG injection. The egg retrieval is usually performed 35-36 hours after the hCG injection is given. We ask that the male partner refrain from sexual intercourse from the time of hCG until after the egg recovery, in order to obtain the best sperm sample possible.
The morning after your hCG injection you will receive final instructions for egg recovery and final medications.

The majority of IVF patients have a sonographic egg recovery performed. This procedure uses ultrasound guidance to retrieve oocytes from your ovaries. The physician places the ultrasound probe into the vagina and guides the aspirating needle through the vagina into follicles on each ovary. Fluid is aspirated from the follicles and transferred to the embryologist, who will identify the eggs under the microscope.
Eggs are cultured and fertilized in the Embryology Laboratory.
During or immediately following the egg recovery, the male partner will need to give a sperm sample. A private room is provided for discrete semen collection. Patients who need to use donor sperm will be given instructions on ordering donor sperm at the time of the initial screening appointment.
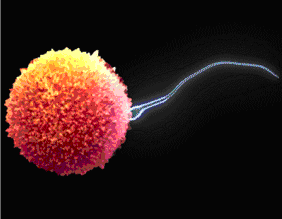
Once the eggs are retrieved, they will be placed in special fluid media for approximately 6 to 12 hours. The semen specimen will be prepared to isolate the best sperm for insemination, then placed with the eggs and incubated overnight. Intracytoplasmic sperm injection (ICSI) may be performed instead for any sperm abnormalities detected.
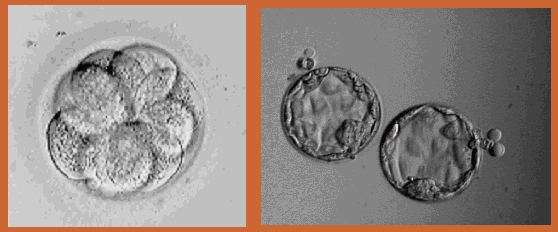
The eggs will then be examined for signs of fertilization, and normally fertilized eggs will be placed into a special growth medium. Embryos will be examined on the third day following insemination. Normally developing embryo(s) will be transferred back into your uterus three to six days after egg recovery, depending on the number and quality of the embryos as they develop in our laboratory.
Not all follicles aspirated can be expected to yield an oocyte. Moreover, all kinds of oocytes can be recovered: mature, immature, and post-mature or degenerate. You will be notified about the number of eggs that have fertilized the day after egg retrieval. Detailed information about the developing embryos will be available at the time of embryo transfer, at which point you will have an opportunity to discuss these results with Dr Frattarelli. Some patients require special therapy such as assisted hatching to enhance implantation of the embryos. These therapeutic options will be discussed in detail with you at your appointments.
This is the return of the embryos that have developed in our laboratory into your uterus. You will lie on an examination table as if you were going to have a Pap smear. There will be no anesthetic required. A very fine soft catheter is placed through the cervix into the uterine cavity under ultrasound observation, and the embryos are transferred inside the uterus through the cervix. Your partner or a friend may be with you during the transfer and during the 15 minute rest period.
The practice of transferring multiple embryos to a woman’s uterus increases her chance for a pregnancy, but also raises the odds of having a multiple birth. The rate of multiple births for ART is higher than that of the normal population. Most of these are twin pregnancies; however, if more than two embryos are transferred, the risk of higher order multiple pregnancies (e.g. triplets) becomes a concern. Multiple pregnancies have increased risks for both mother and babies, particularly preterm delivery.
You will speak to Dr. Frattarelli about your chances of pregnancy and risk for multiple pregnancy. Together, you can determine the appropriate number of embryos to transfer (usually one to three) depending on your personal medical situation.
Depending on your personal medical situation and the quality and number of embryos, you will have the option of cryopreserving (freezing) the remaining embryos for thawing and replacement at a later time.
You will need to have a pregnancy test 10-12 days after the embryo transfer. We recommend the pregnancy test and first obstetric ultrasound (if applicable) be done with our practice. We are also anxious to know the outcome of your cycle, and are better able to offer medical and emotional support if we are informed right away.
Once pregnancy has been confirmed to be doing well with the ultrasound and bloodwork, we will send you back to your referring physician for continue obstetrical care or, if you do not have one, we can provide names of excellent general obstetrician/gynecologists in your area.
Unfortunately not all ART cycles result in pregnancies, you are encouraged to arrange a follow-up appointment with your original and primary physician. This appointment may be done by phone or face-to-face. The purpose of this visit would be to summarize your cycle, answer questions, and discuss future plans, such as future ART cycles, other infertility options or non-medical family building options.
Unfortunately, neither conception nor a successful outcome of pregnancy is guaranteed by the IVF-ET procedure. There are many reasons why pregnancy may not occur with the IVF-ET procedure. In fact, there are complex and largely unknown factors that limit pregnancy rates following assisted reproductive techniques. Some of the known reasons for failure may include, but are not limited to:
Advanced Reproductive Medicine & Gynecology of Hawaii
Helping to Create New Beginnings