A thorough evaluation of infertility also includes male fertility testing. Evaluation and treatment options for male infertility are available at all our practice locations including Honolulu, Kailua, Hilo, Kona, and Kahului.
The male reproductive system is also under the influence of hormones and is responsible for producing sperm. The same hormones that regulate female reproductive functions also regulate the production of sperm in the male. FSH stimulates sperm production, and LH stimulates the production of the hormone testosterone. Testosterone helps maintain sperm production, sexual desire, and male characteristics such as hair growth.
Sperm is produced by the testes (or testicles). The scrotum protects the testes and maintains a constant temperature, which is somewhat lower than normal body temperature, to help sperm develop properly. As sperm are produced, they pass from the testes through the coiled channels of the epididymis, which is an organ that stores and nourishes sperm as they mature.
Once sperm are completely mature (spermatozoa), they move into the vas deferens. This tubal structure connects the epididymis with the seminal vesicles, which are two pouchlike glands that store mature sperm. The entire process of sperm formation to maturation takes about 72 days. However, this is an ongoing process, and sperm are being manufactured all the time.
When a man ejaculates (releases fluid from his penis during intercourse), the sperm from the seminal vesicles combine with a thick fluid from the prostate gland to create semen. The fluid (ejaculate) is deposited into the woman’s vagina. Sperm can live 48 – 72 hours within the female reproductive tract, retaining the ability to fertilize an egg. This is why sexual intercourse around the time of ovulation is necessary for conception to occur.
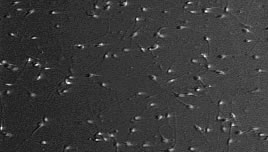
Several factors determine whether a man’s sperm can fertilize an egg. Semen quality and quantity may affect the ability of sperm to fertilize the egg successfully. The ability of sperm to move referred to as motility, appears to be one of the most important factors in determining the fertilizing capability of sperm. Even with a low sperm count, men with highly motile sperm may still be fertile. The shape of the sperm referred to as morphology, may also affect its ability to fertilize an egg. In addition, the sperm must live long enough to reach the egg, a characteristic known as viability.
Infertility is a couples’ problem. Most studies suggest that problems with the male account for about 40 % of all infertility, while couples with problems with both partners’ account for another 20%. The basic test to evaluate fertility in the male is the Semen Analysis.
The purpose of the semen analysis is to:
Based on the results of the semen analysis, recommendations on further evaluation and/or therapy may be made.
The most accurate semen analysis is the one that has been produced at the lab and evaluated promptly. We strongly urge you to produce the specimen at our facility if at all possible. However, we understand that this is not feasible for all couples. Please follow the instructions below for home collections:
At its most basic level, the infertility work-up is trying to determine the optimal method of delivering sperm to the egg. There are 4 ways to deliver the sperm to the egg: (1) intercourse, (2) artificial insemination, (3) in vitro fertilization (IVF), and (4) IVF using intracytoplasmic sperm injection (ICSI).
The semen analysis results are interpreted within the context of the couple’s entire evaluation to provide the most efficient and effective means of sperm delivery for a given situation.
| Volume: 2.0-5.0 cc | If the volume is too small, there may not be enough to get to the cervix, if there is too much, it may dilute the sperm. |
|---|---|
| Concentration: >20 million/cc |
Sperm concentrations may vary widely from within the same individual. Among the factors that can effect the concentration include frequency of ejaculation, environmental factors, surgery/trauma, heat, and ingestibles (drugs, alcohol, and recreational drugs). About 20-25% of fertile men actually have counts below 20 million. |
| Motility: 50% |
This is the proportion of sperm that are swimming. They may swim very fast, moderately fast or slow. The sperm may also wiggle in place or not move at all. |
| Morphology: | The overall appearance of the sperm. The normal range of morphology depends on the laboratory analysis. Please consult with your physician concerning the result. |
| White Blood Cells: < 1 million/cc |
The presence of WBC suggests that an inflammatory process is ongoing in the male reproductive tract. They can secrete factors that inhibit a sperm’s ability to move and fertilize an egg. White blood cells may be markers for infection, which can be treated with antibiotics. |
Men have the benefit of being able to continuously produce sperm (in contrast to a woman being limited to 300-400,000 oocytes that she is born with). This allows men to make behavioral changes that might improve sperm quality. A variety of chemicals are used by men that can adversely affect sperm production and/or function. These include alcohol, marijuana, cocaine, cigarette smoke, and narcotics. For the occasional user of these substances, stopping their use can result in improved semen parameters in 3-6 months for some men.
However, long-term use can result in permanent impairment. A number of drugs also contribute to problems with sperm. These include calcium-channel blockers (anti-hypertensives, see list below), cimetidine, spironolactone, nitrofurantion, sulfasalazine, erythromycin, tetracycline, and anabolic steroids. Other drugs that can be problematic include chromium picolinate, DHEA, ansdrostendione, colchicines, methotrexate and niradazole. Calcium –channel blockers are particularly important to know about, as the sperm can appear normal, but not be able to fertilize an egg because of changes induced in the sperm cell membrane by the medicine.
Chemical exposures by other means can affect sperm production/function. These include heavy metals (lead, mercury, boron), organic solvents (acetone, ethylene glycol, benzene, toluene, etc) and pesticides (dibromochloropropane, ethylene dibromide, carbaryl, chordecone,). Other physical factors that have been associated with sperm abnormalities or reduced fertility include, heat, vibration (truck driving, bike riding), electromagnetic fields and microwave radiation. Therapeutic interventions might include the use of artificial insemination, donor insemination, in vitro fertilization or intracytoplasmic sperm injection with IVF.
Calcium Channel Blockers. Some of the available calcium channel blockers are listed below. If you are on one of these drugs, it is important to tell your doctor and nurse. Calcium channel blocker can alter the sperm cell membrane so that they cannot fertilize an egg, despite being normal in every other way. If you are not sure about one of your medications, please ask your doctor or nurse.
| Generic Name | Brand Name |
| Amlodipine | Norvasc |
| Bepridil | Vascor |
| Diltiazem | Cardizem, Tiazac |
| Felodipine | Plendil |
| Nicardipine | Cardene |
| Nifedipine | Adalat, Procardia |
| Nimodipine | Nimotop |
| Nisoldipine | Sular |
| Verapamil | Calan, Covera, Isoptin, Verelan |
In approximately 40% of infertility cases, abnormalities of the sperm are found. These can include decreased numbers of sperm (oligospermia), decreased sperm motility (asthenospermia) or an unusually high number of abnormally shaped sperm (teratospermia). Some of the common causes of infertility include:
Previous Cancer Treatment: Chemotherapy and radiation can cause abnormal sperm or sterility.
DES (diethylstilbestrol) exposure prior to birth: Synthetic estrogen used in the 50’s and 60’s used by women to prevent miscarriage. Can cause low sperm counts, decreased sperm motility, abnormal sperm forms, abnormally small penis size, undescended testicles (risk factor for testicular cancer), and abnormal testicles.
Hormonal imbalances: Hormone problems affecting sperm count include thyroid problems, low testosterone levels, elevated FSH, and excess prolactin (see next entry).
Immune problems: Immune reactions to sperm in the man (autoimmune) can be a problem post-vasectomy, but may also have other causes. Anti-sperm antibodies can “attack” the sperm, thus preventing it from being able to fertilize the egg.
Impotence/ Sexual Dysfunction: There are a variety of medical causes that can contribute, including diabetes mellitus, medications such as antidepressants, etc. Viagra, according to the manufacturer, does not appear to have any negative impact on sperm. Up to 20% of men may have decreased sexual desire, inability to maintain an erection, and premature ejaculation. This could result from low testosterone or performance anxiety.
Infection: Mumps contracted after childhood and, occasionally, venereal diseases such as gonorrhea and chlamydia can harm male fertility. Also, recurrent infections of the prostate can lower sperm count and motility.
Genetic Abnormalities: A small percentage of infertile men have Klinefelter’s Syndrome; they have two X chromosomes and one Y chromosome, rather than the normal one X and one Y. They are generally tall and thin, with small testicles.
Lifestyle factors:
Obstruction/Blockage: due to prior surgery or infection the vas deferens may be damaged.
Previous Vasectomy: Vasectomies can often be reversed. However, the more time has passed, the more likely it is that the man will have an immune reaction to his own sperm and the lower the chance of being able to produce a pregnancy.
Retrograde ejaculation: Can be caused by certain medications, surgeries, and nerve damage (for example, from diabetes mellitus). Sperm goes in the wrong direction and is ejaculated into the bladder.
Trauma to testicles: Severe injury to the testicles can result in decreased sperm production.
Varicocele: An enlarged vein in the scrotum, which causes pooling of blood and an elevated temperature. Although controversial, some argue it is one of the most common and readily treatable causes of male infertility. Others say that varicocele is also common among fertile men, and question the connection with infertility and the need for treatment. In general, very large or painful varicoceles that go untreated can cause permanent damage to the testicles. These should be surgically treated.
Sperm is carefully washed and prepared so that the most motile and viable sperm are concentrated into a very small volume to be injected into the uterine cavity. Searching through about a dozen medical journal articles and a number of web sites resulted in a rather wide-range of statistics. Basically, the odds of success are reported to be as low as just under 8% and as high as 26% per cycle. The low statistics are with one follicle, while multiple follicles resulted in as high as 26% success. Another influencing factor is sperm count. Higher sperm counts increase the odds of success, however, there was little difference between success with good-average counts and those with high counts. The overall success rate seems to be between 15-20% per cycle based on the current literature. The rate of multiple gestation pregnancies was 23-30%.
The option of using donor sperm has been available to couples with severe male infertility for a long time now. While the addition of ICSI can treat almost all severe male factor infertility, some couples may choose to use donor sperm from one of many certified sperm banks across the country due to concerns of genetic disorders that affect sperm production (like Cystic Fibrosis). Once a donor is chosen, the sperm is washed and prepared in a similar fashion to that of an IUI.
Advanced Reproductive Medicine & Gynecology of Hawaii
Helping to Create New Beginnings