Infertility is a couple’s problem. Most studies suggest that problems with the male account for about 40% of all infertility, while couples with problems with both partners account for another 20%. The basic test to evaluate fertility in the male is the Semen Analysis.
The purpose of the semen analysis is to:
Based on the results of the semen analysis, recommendations on further evaluation and/or therapy may be made.
Note: A physician’s order or consult with Dr. Frattarelli or Dr. Karmon is need prior to scheduling.
The most accurate semen analysis is the one that has been produced at the lab and evaluated promptly. We strongly urge you to produce the specimen at our facility if at all possible. However, we understand that this is not feasible for all couples. Please follow the instructions below for home collections:
At its most basic level, the infertility work-up is trying to determine which is the optimal method to deliver the sperm to the egg. There are 4 ways to deliver the sperm to the egg: (1) intercourse, (2) artificial insemination, (3) in vitro fertilization (IVF), and (4) IVF using intracytoplasmic sperm injection (ICSI).
The semen analysis results are interpreted within the context of the couple’s entire evaluation to provide the most efficient and effective means of sperm delivery for a given situation.
| Volume: 2.0-5.0 cc | If the volume is too small, there may not be enough to get to the cervix, if there is too much, it may dilute the sperm. |
|---|---|
| Concentration: >20 million/cc |
Sperm concentrations may vary widely from within the same individual. Among the factors that can effect the concentration include frequency of ejaculation, environmental factors, surgery/trauma, heat and ingestables (drugs, alcohol, recreational drugs). About 20-25% of fertile men actually have counts below 20 million. |
| Motility: 50% |
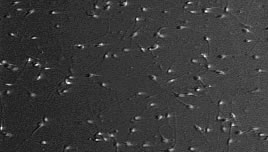
This is the proportion of sperm that are swimming. They may swim very fast, moderately fast or slow. The sperm may also wiggle in place or not move at all. |
| Morphology: | The overall appearance of the sperm. The normal range of morphology depends on the laboratory analysis. Please consult with your physician concerning the result. |
| White Blood Cells: < 1 million/cc |
The presence of WBC suggest that an inflammatory process is ongoing in the male reproductive tract. They can secrete factors that inhibit a sperm’s ability to move and fertilize an egg. White blood cells may be markers for infection, which can be treated with antibiotics. |
Men have the benefit of being able to continuously produce sperm (in contrast to a woman being limited to 300-400,000 oocytes that she is born with). This allows men to make behavioral changes that might improve sperm quality. A variety of chemicals are used by men that can adversely affect sperm production and/or function. These include alcohol, marijuana, cocaine, cigarette smoke, and narcotics. For the occasional user of these substances, stopping their use can result in improved semen parameters in 3-6 months for some men.
However, long-term use can result in permanent impairment. A number of drugs also contribute to problems with sperm. These include calcium-channel blockers (anti-hypertensives, see list below), cimetidine, spironolactone, nitrofurantion, sulfasalazine, erythromycin, tetracycline, and anabolic steroids. Other drugs that can be problematic include chromium picolinate, DHEA, ansdrostendione, colchicines, methotrexate and niradazole. Calcium-channel blockers are particularly important to know about, as the sperm can appear normal, but not be able to fertilize an egg because of changes induced in the sperm cell membrane by the medicine.
Chemical exposures by other means can affect sperm production/function. These include heavy metals (lead, mercury, boron), organic solvents (acetone, ethylene glycol, benzene, toluene, etc) and pesticides (dibromochloropropane, ethylene dibromide, carbaryl, chordecone). Other physical factors that have been associated with sperm abnormalities or reduced fertility include, heat, vibration (truck driving, bike riding), electromagnetic fields and microwave radiation. Therapeutic interventions might include the use of artificial insemination, donor insemination, in vitro fertilization or intracytoplasmic sperm injection with IVF.
Below are listed the calcium-channel blockers that are listed below from the 2001 PDR. If you are on one of these drugs, it is important to tell your doctor and nurse. Calcium-channel blocker can alter the sperm cell membrane so that they cannot fertilize an egg, despite being normal in every other way. If you are not sure about one of your medications, please ask your doctor or nurse.
| Generic Name | Brand Name |
| Amlodipine | Norvasc |
| Bepridil | Vascor |
| Diltiazem | Cardizem, Tiazac |
| Felodipine | Plendil |
| Nicardipine | Cardene |
| Nifedipine | Adalat, Procardia |
| Nimodipine | Nimotop |
| Nisoldipine | Sular |
| Verapamil | Calan, Covera, Isoptin, Verelan |
Advanced Reproductive Medicine & Gynecology of Hawaii
Helping to Create New Beginnings